Project completed as part of the South Health Campus, Alberta Health Services Green Team Competition, 2024
Team members
- Julia MacLaren (Wellness Kitchen Consultant, South Health Campus)
- April Matsuno (Wellness Centre Manager, South Health Campus)
Setting / patient group: Oncology patients
Issue
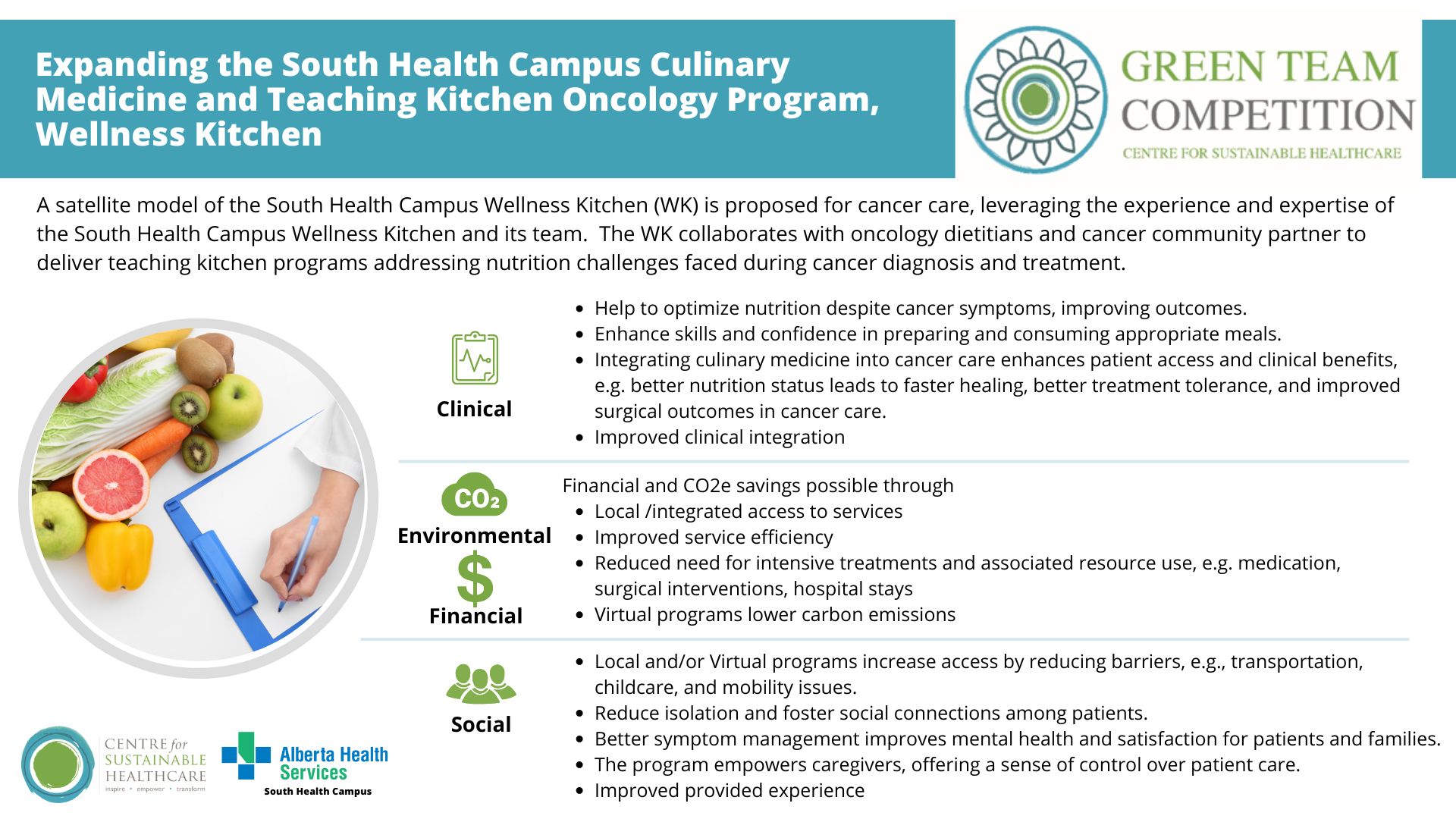
Cancer patients often face challenges achieving and maintaining optimal nutrition status, which is a predictive factor of prognosis, in terms of morbidity and mortality, and impacts the frequency and intensity of other oncology interventions needed to optimise care (including treatments, hospital stays, and physician services). An underutilized intervention in Alberta’s oncology care system, Culinary Medicine (CM) and Teaching Kitchens (TK) offer a practical, evidence-based approach for patients and caregivers to develop confidence, self-efficacy, and needed food preparation skills to applying evidence-based nutrition care recommendations.
Intervention
The South Health Campus Wellness Kitchen, the only operational TK in Alberta Health Services (AHS), is broadcast media equipped to serve the entire province of Alberta. In partnership with clinical teams, it provides CM programs for patients and families helping them translate evidence-based nutrition guidance to ‘the plate’ through practical food skills training and recipe and meal-based examples. The “Cancer Recovery for People with Eating Challenges” South Health Campus Wellness Kitchen program is currently offered in collaboration with clinical dietitians and a community partner organization, to improve the health outcomes of cancer patients by addressing nutrition challenges. Expanding this model to a satellite TK at an AHS Cancer Centre and integrating CM into oncology care pathways is proposed to promote prevention, self-care, lean clinical pathways, and low-carbon alternatives.
Potential impacts
Clinical: CM interventions can improve cancer patients’ nutrition status through improved self-efficacy, confidence and food skills to implement dietary change. Through reduced treatment side effects and symptoms and improved tolerance to oncology therapies, patients with optimised nutrition care during cancer have better surgical outcomes, reduced hospital stays, and improved cancer morbidity and mortality outcomes. Integrating CM into cancer care pathways also boosts clinician awareness and increases referral rates, enhancing patient access.
Environmental: Any capacity to reduce intensive treatments like surgical revisions, medication use, and hospital stays translates into significant carbon savings. As one small-scale theoretical example, improving patients’ ability to manage nausea during chemotherapy through optimised nutrition care with CM reduces the amount of needed antiemetic medicines. If just one dose of Olanzapine was prevented in 1,000 patients, throughout their entire course of treatment, CO2e emissions would be reduced by over 13,569 kgCO2e – equivalent to driving from Calgary, AB to Fredericton, NB. Virtual CM classes further reduce emissions through decreased patient travel, and co-location and integration of in-person programs reduces patient and clinician travel between sites, while optimizing use of already-built structures.
Social: CM programs foster a sense of community and reduce feelings of isolation for cancer patients and their families/caregivers and are frequently requested. Caregivers gain confidence in managing patients’ nutritional needs, improving both patient and family well-being. Clinicians benefit from enhanced therapeutic approaches to symptom management and ability to meet patient and family requests with practical interventions. Virtual sessions also provide more equitable access to care for rural patients and those facing mobility or logistical challenges.
Financial: The long-term financial savings of CM programs are substantial. Improving surgical outcomes, reducing the amount of medications needed for symptom management, or shortening hospital stays, for example, all result in lower healthcare costs. Building on the environmental example, reducing Olanzapine use by one dose each in 1,000 patients could save $18,790 CAD. Additionally, the efficient use of TK spaces and virtual programming minimizes operational costs while expanding patient reach.
Key Learning Point
Leveraging the operational efficiencies, skill set, experience, and expertise of the Wellness Kitchen team and its clinical partners, a satellite model of operations to establish a CM strategy in cancer care has significant potential to improve clinical integration, timely patient access to oncology-specific CM cancer care, and improve experiences and outcomes for cancer care patients and their caregivers. The satellite model aligns with the Centre for Sustainable Healthcare principles of sustainable practice, offering opportunities for prevention, patient empowerment and self-care, lean clinical pathways, and low carbon alternatives to improve all parameters of the triple bottom line of sustainability in cancer care in Alberta.
Please log in or sign up to comment.