Project completed as part of the South Health Campus, Alberta Health Services Green Team Competition, 2024
Team members
- Sean Sloan, BSc, BScPT - Program Facilitator
- Tracy Smith, BSW, MSW, RSW - Social Work Clinical Practice Leader
- Shauna Thomas, BSc. O.T.(c), MClSc.W.H. - Occupational Therapist Clinical Practice Leader
- Nancy Egbogah, RN, MN - Hospitalist Liaison Nurse
- BSW, RSW - Inpatient Social Workers
Setting / patient group:
Inpatient setting. Patients requiring pre-capacity assessment prior to discharge either to home or a disposition location.
Issue:
The team identified that the pre-capacity assessment process and MDT collaboration could be optimised to improve patient care.
Intervention
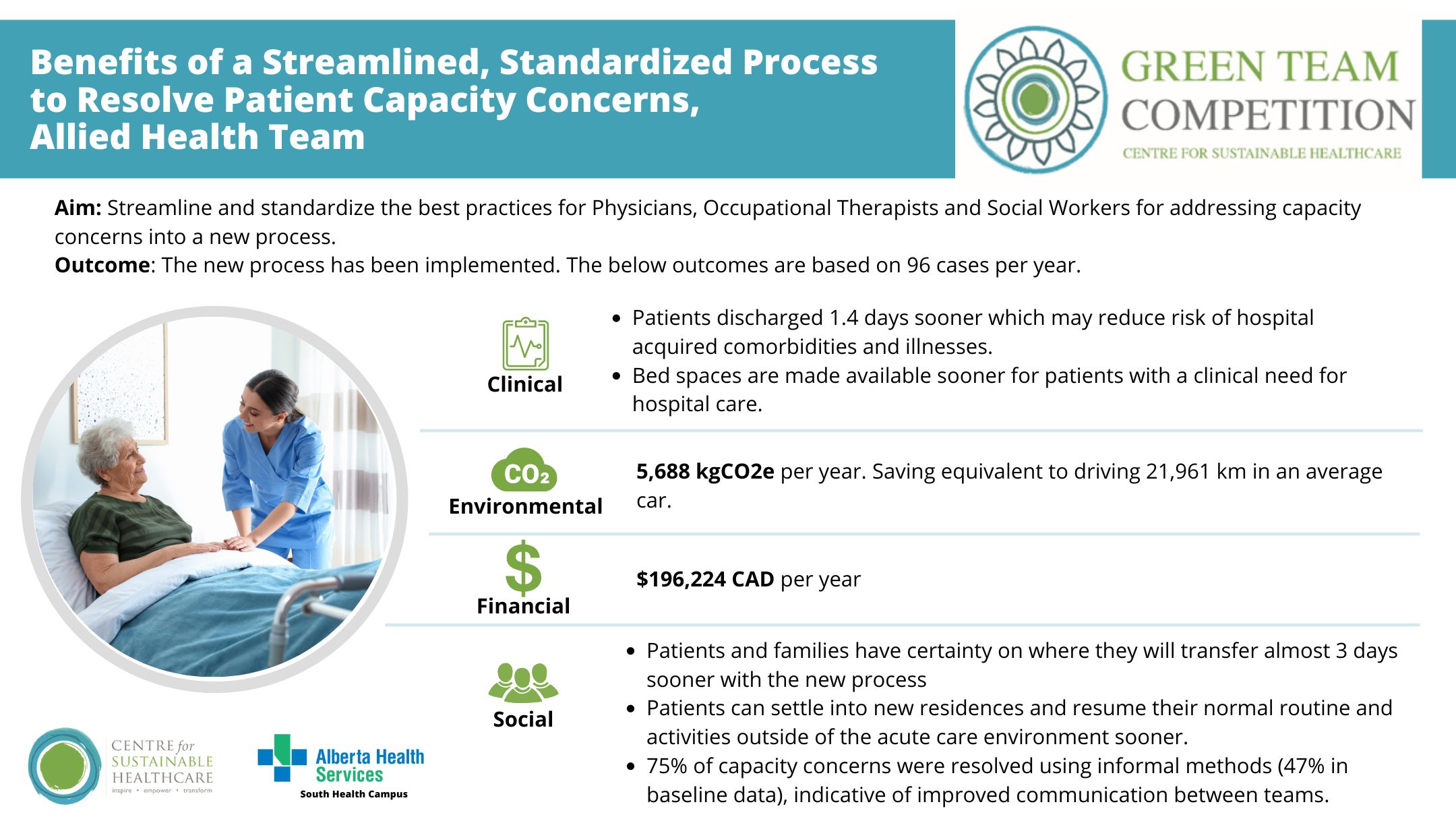
The project aimed to streamline and standardize the best practices for Physicians, Occupational Therapists and Social Workers for addressing capacity concerns into a new process.
The team evaluated their current process and identified inconsistencies and barriers to find opportunities for improvement. Several changes were made including standardising assessment orders and use of SmartPhrase, developing a process for communicating results of pre-capacity assessments through electronic messaging, developing a workflow/decision tree identifying clear alternatives to formal pre-capacity assessments and education to physicians, OT’s and SW’s regarding the importance of ongoing and regular communication to guide them through the pre-capacity assessments process.
Outcomes
Patient outcomes:
- Patient capacity concerns were resolved using informal methods in 75% of cases in our project cohort compared to 43% of cases in our baseline sample.
- Pilot results show patients were discharged 1.4 days sooner compared to baseline data.
- 75% of pre-capacity assessments had a new OT and SW order placed when the physician determined a pre-capacity assessment was required.
- Use of the Smartphrase in the pre-capacity orders improved to 75% (3 of 4 cases) from baseline of 31%.
Environmental sustainability:
Based on the change being applicable to 96 patients per year, 5,688 kgCO2e will be saved, equivalent to driving 22,000 kms.
Economic Sustainability:
Annual financial savings are estimated to be $196,224 of reallocated beds to acute care patients.
Social sustainability:
Patients and families: With the new process, patients and families had certainty on where they were going to transfer to almost 3 days sooner. Patients were discharged 1.4 days faster allowing patients to settle into their new residences sooner, resume normal routine and activities outside of the acute care environment. Reduces length of stay may reduce risk of hospital acquired comorbidities and illnesses.
Staff: Our project demonstrated 75% of capacity concerns were resolved using informal methods, as compared to 47% in our baseline data. This is highly indicative of improved communication between the teams, leading to fewer inappropriate requests for formal pre-capacity assessment.
Key learning point
Success of this project was driven by strong engagement from our physician group along with our occupational therapists and social workers. PDSA cycles allowed us to implement, then adjust our resources and education to support our team as we rolled out the new process.
Please log in or sign up to comment.