Project completed as part of the Calgary Zone, Alberta Health Services Green Team Competition, 2025
Team members
- Dina Fisher – Respiratory Physician Lead PLC
- Joel Chen – Respiratory Physician PLC
- Dawn Papp – PLC Respiratory Services, Pulmonary Diagnostics Supervisor
- Alan Sutton – PLC Respiratory Services, Pulmonary Diagnostics Manager
- Claire Barber – Associate Vice Chair Planetary Health DOM
- Arooj Nazir – Quality & Process Improvement Consultant
- Kiran Dhiman – Research Coordinator & Precision Health Student in Quality Improvement and Safety Health Leadership
- QI Group: Jelena Poprzen, Monica Veness – Clinical Quality Improvement Consultants
- Omenaa Boakye – Lead, Provincial Projects-Acute Care Alberta
Setting: Outpatient pulmonary function testing (PFT) lab
Issue:
Pulmonary function testing (PFT) often requires bronchodilator responsiveness (BDR) testing using a short-acting bronchodilator, typically salbutamol (Ventolin) via metered dose inhaler (MDI). In all Calgary Zone hospital-based PFT labs, a single-use Ventolin MDI is used per patient, delivering only 4 puffs. Some of these inhalers are subsequently provided to the patient, if desired and deemed appropriate by their treating physician. However, many are discarded with approximately 98% of the medication remaining. This practice results in significant waste and environmental impact, especially given the high carbon footprint of each inhaler, despite many patients potentially having their own prescribed inhalers suitable for testing.
Intervention:
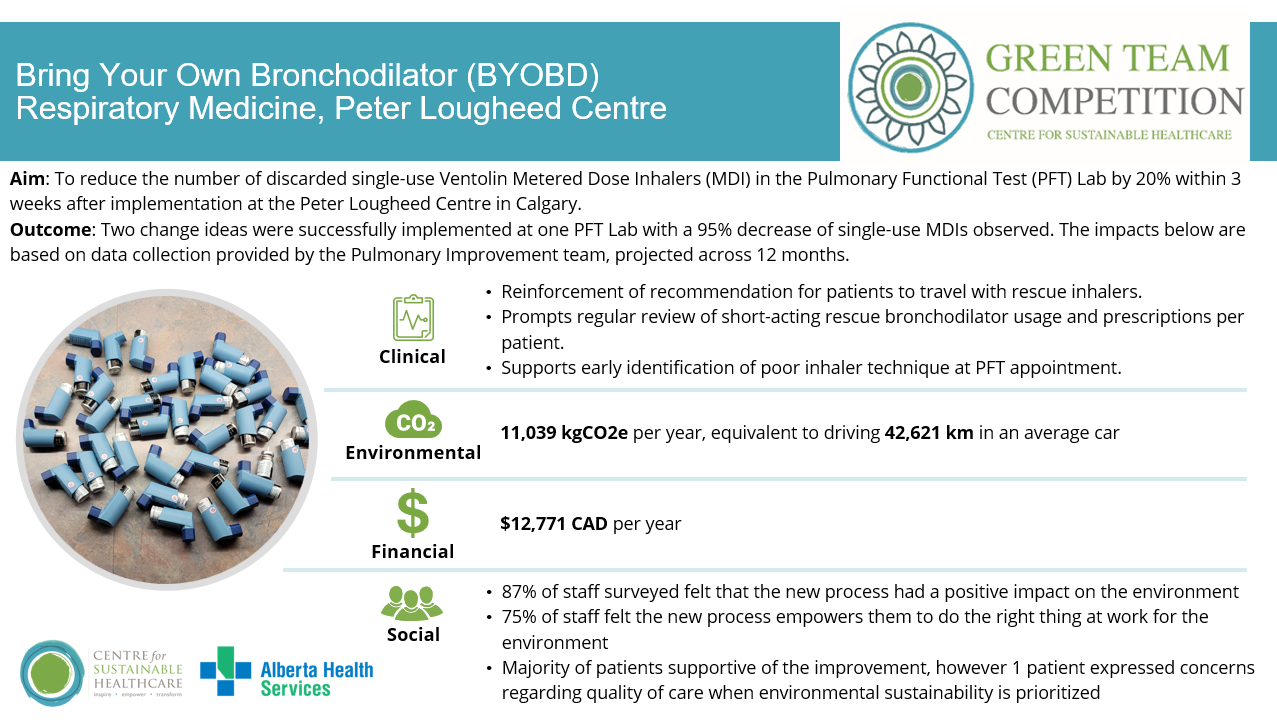
Aim: To reduce the number of discarded single-use Ventolin Metered Dose Inhalers (MDI) in the Pulmonary Functional Test (PFT) Lab by 20% within 3 weeks after the implemenattion at the Peter Lougheed Centre in Calgary.
The first change was the development of a protocol allowing patients to use their own prescribed short-acting bronchodilator for BDR testing in the PFT lab. This involved reviewing respiratory literature to confirm appropriate dosing for various inhalers, creating a written guide for staff, and implementing a reminder system for patients to bring their inhalers to appointments. Staff orientation and management approval were completed within 8 weeks.
The second change was to discuss opportunities for multi-patient use of MDIs. This involved meetings with Infectious Disease Physician Lead and Infection Prevention and Control practitioners. With this protocol change Ventolin MDIs in the PFT lab could be used for up to 50 patients. This required stakeholder engagement, protocol and recommendation development, and staff training over a 10-week period, and was implemented two weeks after the first intervention.
Outcomes:
Clinical:
No specific measurement was included for this project. Reported benefits from respiratory therapy staff, respiratory physicians, asthma/COPD educations include:
• Reinforcement of recommendation for patients to travel with rescue inhalers.
• Prompts regular review of short-acting rescue bronchodilator usage and prescriptions per patient.
• Supports early identification of poor inhaler technique at PFT appointment.
Environmental:
In our baseline count over 7 weeks of study prior to implementation of any initiative, 23 MDIs were being discarded at the PLC PFT lab per week, including 23 holding chambers per week. This was reduced to 1.25 Ventolin inhalers and 10 holding chambers per week with both interventions implemented.
Across one year this is a saving of 11,039 kgCO2e per year, equivalent to driving 2,859 km in an average car (a round trip from Calgary, Alberta to Denver, Colorado).
The PFT lab in the 3 other acute care sites in the Calgary Zone, have also implemented this intervention. Assuming similar PFT test utilization numbers (as all acute care PFT labs are booking at
full capacity), the projected savings over one year of implementation at all 4 sites would be estimated at 44,154.24 kgCO2e.
Financial
$12,771CAD per year savings in PFL at Peter Lougheed Centre
With the expansion to all 4 adult acute care sites in the Calgary Zone, $51,086CAD could potentially be saved per year
Social
• 87% of staff surveyed felt that the new process had a positive impact on the environment
• 75% of staff felt the new process empowers them to do the right thing at work for the environment
• Majority of patients supportive of the improvement, however 1 patient expressed concerns regarding quality of care when environmental sustainability is prioritized
Key learning point
The initiative was supported by multiple stakeholders, including the AHS Green Team and Department of Medicine, and is now being expanded across the Calgary Zone. When barriers were identified, having the highly motivated team members/local champions assist with explaining the importance of this intervention supported protocol progress and buy-in from all stakeholders.
Please log in or sign up to comment.