Project completed as part of the Calgary Zone, Alberta Health Services Green Team Competition, 2025
Team members
Alaina Bosinski (Patient Care Manager), Candice Horbay (Unit Manager), Amber Martin (Clinical Nurse Educator), Dr. Heidi O’Grady (Infection Control Professional), Dr. John Conly (Infectious Diseases Physician), Nikita Baker (Quality Improvement Consultant), Sheena Hammond (Quality Improvement Consultant), Kevin Huntley (Pulmonary Nurse Practitioner), Mohamad Hlaihel (Nurse Clinician), Kathleen Lowe (Nurse Clinician), Pamela Schmidt (Nurse Clinician), Dr. Byron Berenger (Medical Microbiologist and Provincial Microbiology Section Chief, APL), Dr. Chris Hergott (Respiratory Medicine Site Lead), and Rachel Rouble (Executive Director)
Setting: Acute care hospital – Primary respirology unit, immunocompetent Coronavirus Disease 2019 (COVID-19) management
Issue:
The current guidance for isolation of immunocompetent COVID-19 positive patients requires contact and droplet precautions for 11 days after symptom onset or the initial positive test date, regardless of symptoms. While isolation and PPE is essential for infection control, it imposes considerable financial costs, time demands, environmental impact, and clinical challenges, along with social and psychological burdens for both patients and the healthcare workers. The unit admits patients with complex medical conditions and sees high patient turnover, making efficient use of limited isolation rooms and staff resources particularly critical.
Although COVID-19 test results are reported as positive or negative, the lab also has access to cycle threshold (Ct) values, which correlates with viral load. Higher Ct values are consistently associated with a lower amount of virus present in the sample. A recent retrospective case series carried out by Infection Prevention and Control (IPC) identified 12 patients who, in the absence of progressive COVID-19 symptoms, underwent follow-up swab testing, with CT values supporting patient de-isolation within 1–4 days compared to the standard 11-day period.
Intervention:
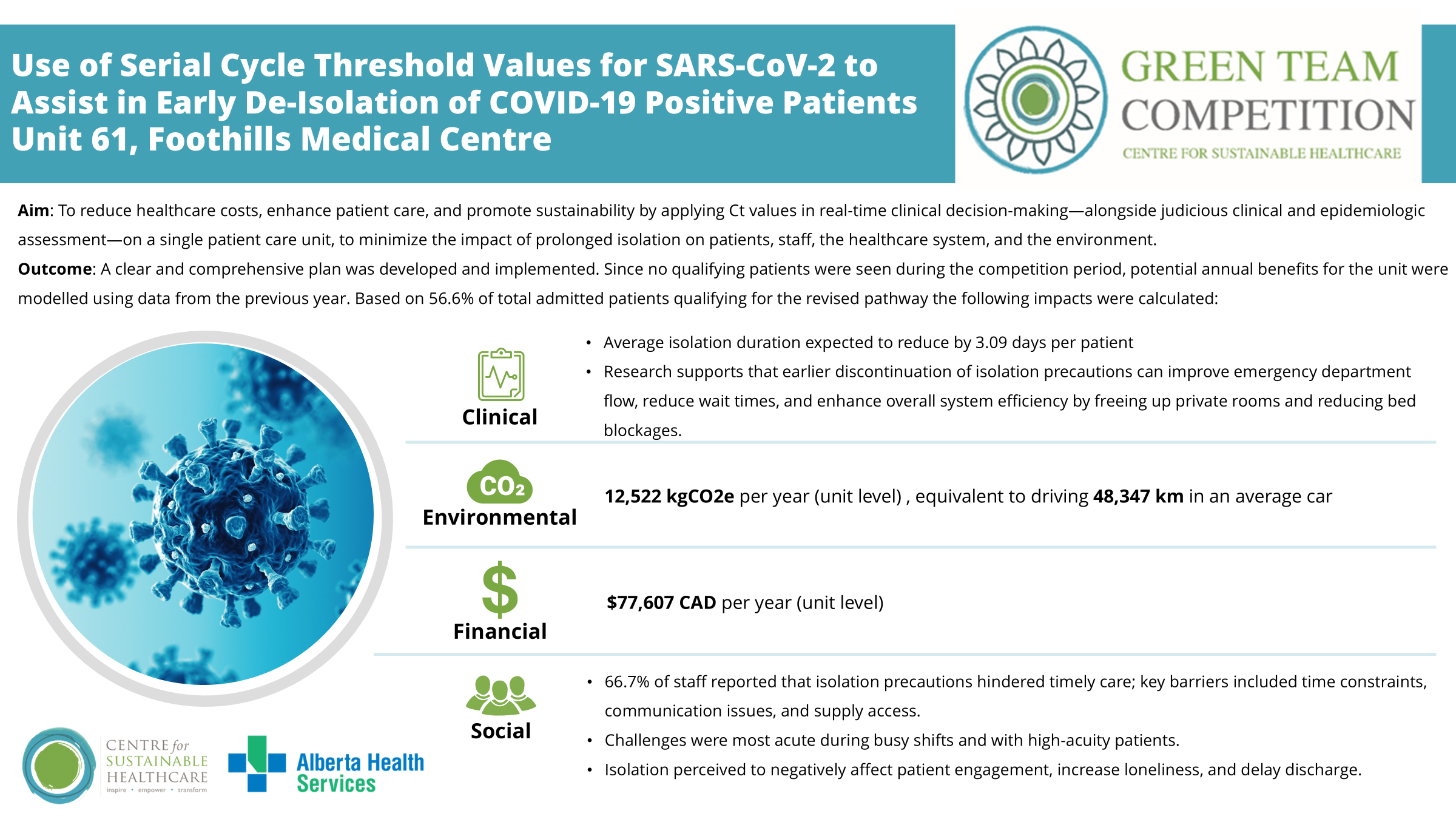
Aim: To reduce healthcare costs, enhance patient care, and promote sustainability by applying Ct values in real-time clinical decision-making—alongside judicious clinical and epidemiologic assessment—on a single patient care unit, to minimize the impact of prolonged isolation on patients, staff, the healthcare system, and the environment.
The team created a new revised process for use of Ct values to aid clinical decision-making. In the new process, Nurse Clinicians and IPC complete a daily review for any new SARS-CoV-2 positive patients and their corresponding Ct values. Clinically stable patients with two swabs showing Ct above 30 would be assessed and, if deemed non-transmissible, have isolation discontinued by the most responsible health practitioner. Supporting tools included an education package and a shared Excel tracker to guide consistent documentation and decision-making.
Outcomes:
A clear and comprehensive plan was developed and implemented. Since no qualifying patients were seen during the competition period, potential annual benefits for the unit were modelled using data from the previous year. Based on 56.6% of total admitted patients qualifying for the revised pathway clinical, environmental, financial and social impacts were calculated:
Clinical:
The average isolation duration for qualifying patients could be reduced by 3.09 days per patient.
Research supports that earlier discontinuation of isolation precautions can improve emergency department flow, reduce wait times, and enhance overall system efficiency by freeing up private rooms and reducing bed blockages.
Environmental and Financial Savings:
Total savings were determined by subtracting the impact of additional COVID-19 swabs from the projected savings gained through reduced PPE usage from reduced isolation days and decreased medication usage.
Total projected unit level annual environmental saving: 12,522 kgCO2e
Total projected unit level annual financial saving: $77,607CAD
Social
Patient feedback regarding experiences while on isolation for COVID-19 infection have described experiences of delayed care, emotional distress, and perceived inequities in service delivery. Comments from patients collected between Jan 2021 and Dec 31, 2022, by the AHS Engagement and Patient Experience Team highlighted issues such as missed meals, long waiting times for assistance, visible staff fatigue, and a general sense of disparities in care.
For staff, a survey indicated that 66.7% felt isolation precautions always or often impacted their ability to provide timely care, compared to 33.3% that felt they were rarely or sometimes impacted. Survey results were categorized into three areas
- Barriers to safe and efficient care in isolation rooms: Staff perceived time constraints, communication breakdowns, and supply issues as barriers to delivering timely and effective care in isolation settings
- Challenging periods during shifts: busy morning shifts or when managing high-acuity patients as especially challenging for donning and doffing PPE.
- Perceived impacts of COVID-19 isolation measures on patient well-being: included reduced engagement in care, increased loneliness, and delays in discharge due to limited mobility and fewer opportunities for education and social interaction.
By reducing isolation days through this QI project, we will be removing the barriers to care and negative outcomes to patients perceived by staff due to isolation.
Key learning point
Key learning from this initiative includes that early identification of partners is critical to successful development and implementation, ensuring alignment and fostering collaboration. The strategic selection of this primary respirology unit, combined with strong interdisciplinary collaboration, ensured a clinically relevant and evidence-informed approach.
The intervention supports more efficient use of isolation resources, reduces unnecessary PPE consumption, and improves care delivery, contributing to system-wide sustainability and resilience. Importantly, the project aligns with Alberta Health Services’ strategic goals of achieving a balanced budget, improving emergency department and acute care flow, and enhancing patient experience.
Please log in or sign up to comment.